By Lynn Schultz-Writsel
While intimate partner homicides have decreased in the past 30 years, women are still nine times more likely to be killed by an intimate partner than by a stranger. The major risk factor for such homicides? Prior domestic violence.
So reports a team of Johns Hopkins University School of Nursing researchers and colleagues in the July 2007 issue of Trauma, Violence & Abuse. The investigators’ findings were based on a review of research conducted over the past 10 years.
In 83% of intimate partner homicide cases, either the victim or the perpetrator had contact with justice, victim assistance, or health agencies in the year prior to the homicide, noted faculty members Jacquelyn C. Campbell, PhD, RN; Nancy Glass, PhD, RN; and Phyllis W. Sharps, PhD, RN, and other researchers.
Other risk factors included gun access, estrangement, threats to kill and threats with a weapon, nonfatal strangulation, and the female victim’s child (perpetrator’s stepchild) living in the home. Unemployment by the male partner was also an important factor.
Also writing in the July issue of Trauma, Violence & Abuse, associate professor Daniel J. Sheridan, PhD, RN, and PhD student Katherine R. Nash, MSN, RN, compiled the mechanisms, locations, and types of injury sustained by women who have survived intimate partner violence. The researchers’ goal: to help health care providers to better differentiate injuries that may have occurred accidentally from those inflicted intentionally.
Sheridan and Nash’s review of the forensic literature indicates that the most common mechanism of IPV injury is being struck with a hand. The head, neck, and face are the most common locations for such injuries. They also observe that strangulation is under-assessed—it is experienced by more than half of IPV victims—and that soft tissue injuries are the most common type of injury suffered.
 New Aid for PhDs
New Aid for PhDs Faced with a Pandemic, “Little Holy One” is Guided by Indigenous Values
Faced with a Pandemic, “Little Holy One” is Guided by Indigenous Values Hill’s Side
Hill’s Side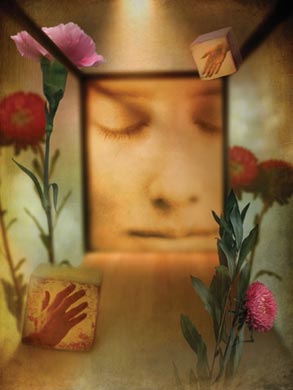 The Worst Fear
The Worst Fear Contributors
Contributors







