Back in May, Bruce Schoneboom wrapped up his appointment to the HHS Pain Management Best Practices Inter-Agency Task Force. The group determined best practices for managing chronic and acute pain—and addressed judicious prescribing of opioids.
If you didn’t know:
- The CDC reports there are 192 overdose deaths in the U.S. every day.
- Forty percent of opioid overdose deaths involved a prescription opioids
- Eighty percent of people who use heroin first misused prescription opioids
And yet we can’t not use them.
Opioid therapy is integral to pain management in many conditions. And barring access can challenge health equity—as is the case in sickle cell disease. So best practices for pain management is a complex—and urgent—concern that needs attention from the nation’s best minds right now.
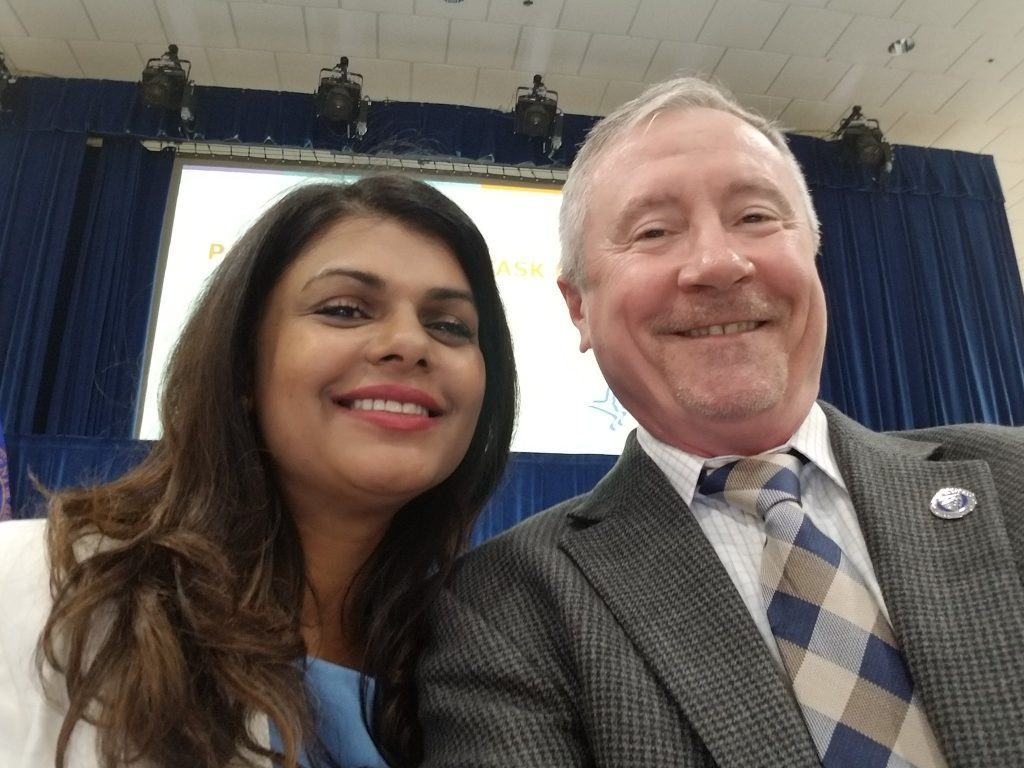
Bruce Schoneboom, PhD, CRNA, FAAN, Associate Dean for Practice, Innovation and Leadership, rose to the challenge. Dr. Schoneboom is a retired army colonel and nurse anesthetist; he’s the power behind the new DNP Nurse Anesthesiology track available at the Johns Hopkins School of Nursing. Read on for Dr. Schoneboom’s reflections on the Task Force.
Can you describe the back story of the Pain Task Force?
It came out of the Comprehensive Addiction and Recovery Act of 2016, signed into law by President Obama. It mandated an interagency task force to determine best practices, recommendations for chronic and acute pain, and recommendation for how to address gaps in pain care.
I was nominated by the American Association of Nurse Anesthetists (AANA) and appointed by HHS Secretary Alex Azar to be one of 29 task force members. We were led by Dr. Vanila Singh, Task Force Chair, Chief Medical Officer, Office of the Assistant Secretary for Health, U.S. Department of Health and Human Services.

What unique perspective do nurse anesthetists bring to pain management?
Nurse anesthetists have unique expertise in chronic and acute pain management. Our role is to administer anesthesia so patients may go through medical procedures in a pain-free or pain managed environment. We understand the neurobiology of pain, how the brain senses it and interprets it, and we have a subspecialty chronic pain management certification.
How to Become a Nurse Anesthetist
What were some key takeaways of the task-force recommendations?
#1 Patient-centered care is key. There’s no “one-size-fits-all” solution to pain.
You’re dealing with a lot of vulnerable populations with unique needs and comorbidities. For example, among veterans that could include post-traumatic stress disorder, traumatic brain injuries, and more.
Comorbid conditions need to be appropriately managed; if not pain experienced will be more intense.
Patient-Centered Care Is Key to Best Practices in Pain Management
#2 We must be aware of potential unintended consequences
Patient advocates were vocal. There is an opioid crisis, yet in our response we can leave behind patients whose conditions require opioid therapy. Then, the CDC’s 2017 Guideline for Prescribing Opioids for Chronic Pain, which intended to help providers prescribe more judiciously, ended with patients force tapered off of medication or abandoned by providers, and their quality of life deteriorated. It drove a large subset of the population to illicit drugs.
Stigma impacts providers too. The CDC guidelines deterred some clinicians from providing care because they felt they were seen as crooks. That’s why these best practices are important; we must provide practitioners with the education they need to be good providers.
How are task force recommendations being translated into practice?
It starts with education, identifying what the best practices are and then getting the word out about them. One of our charges was a dissemination plan. We’re talking about it at professional meetings, I’ve spoken about it at AANA.
We sent the report to congress. We’re waiting to hear if there will be congressional hearings. And we are working with policy makers to make sure we develop good policy based on our recommendations.
What was it like to represent nurses on the task force?
I am honored to serve my country. I was nominated by the AANA to represent over 54,000 nurse anesthetists across the country. But I showed up on day one and realized I was the only registered nurse, too, so I felt a larger obligation to be the voice for the 4 million nurses in the U.S. I applaud Dr. Vanila Singh for including me.
It was challenging to get the narrative away from diagnosis and treatment, from focus on disease to a patient centered approach that is multidisciplinary and multimodal, using a variety of approaches. There was also a dentist, a social worker, a clinical psychologist, and an addiction specialist. We banded together to promote inclusive language in the recommendations, too.
It was a great responsibility to make sure all nurses’ voice are represented. I am thankful for the opportunity to do so, and honored to represent Johns Hopkins and the American Association of Nurse Anesthetists.
Learn more:
- DNP Nurse Anesthesia Track
- How to Become a Nurse Anesthetist
- Pain Management Best Practices Inter-Agency Task Force
- Patient-Centered Care Is Key to Best Practices in Pain Management
- Believe Me When I Say That I’m In Pain
- Communities That Care

ABOUT THE AUTHOR: SYDNEE LOGAN
Sydnee Logan is the Social Media and Digital Content Coordinator for Johns Hopkins School of Nursing. She shares what’s going on with the world.

 RNs, Nurse Practitioners, and Nurse Anesthetists Are Among U.S. News & World Report’s Top 10 ‘Best Health Care Jobs’
RNs, Nurse Practitioners, and Nurse Anesthetists Are Among U.S. News & World Report’s Top 10 ‘Best Health Care Jobs’ Meet the First Cohort of the DNP Advanced Practice Nurse Anesthesia Track
Meet the First Cohort of the DNP Advanced Practice Nurse Anesthesia Track Nurse anesthetists: Leading the way in DNP education
Nurse anesthetists: Leading the way in DNP education CRNA: Living the Dream
CRNA: Living the Dream Open to All
Open to All







