Interview by Catherine Gara
Q&A with nurse and president of Johns Hopkins Health System
Kevin Sowers, MSN, RN, FAAN, is the president of the Johns Hopkins Health System and executive vice president of Johns Hopkins Medicine. He comes from Duke University Hospital, where he worked for 32 years, including the last eight as president and CEO. He was asked the following questions at a press conference in December and an interview in March.
Why did you decide to become a nurse?
I grew up on a farm in rural Ohio and no one in my family had ever gone to college. I started in voice and piano. Because my family grew up below the poverty line, we did not have the resources to pay for me to go to college. So, I worked two jobs—in the morning I would go to the county nursing home and do music therapy. In the afternoon I was an orderly, bathing people and putting them to bed. It was in those summer months I really found my passion for caring for human beings. While I was in nursing school my grandfather was diagnosed with glioblastoma. It was a difficult diagnosis with a difficult outcome. I remember our family did not have the best experience, so I wanted to be a nurse to make sure no other family went through what we went through.
What does your new position involve?
I’ll give you broad strokes. As president of the Johns Hopkins Health System, I’m responsible for the overall performance of the health system. That includes quality and safety, work culture, patient experience and financial performance, and all four of those pillars are important.
As executive vice president of Johns Hopkins Medicine, I partner with leadership to assure that all the decisions we make support our missions of clinical care, education, and research. We have to balance what we do on the health system side to ensure that we can support research and education on the school side.
How does your training as a nurse help you?
I know what it means to take care of a patient, to deliver care. And I know the models that have to be put together to be able to sustain that. I come from the front line and there’s a great value to that in my leadership role. I draw upon it often.
Do you miss the bedside?
There is something I miss. When I was seeing patients, I would go home from my shift knowing what I had done to make a difference in somebody’s life. In executive roles, the outcomes don’t come as quickly and you have to really be patient while bringing people along a journey of transforming an organization.
One third of newly licensed RNs leave the field after just two years. How can we turn that around?
The issue of burnout and resilience is a health care provider issue; it’s not just nurses. There are multiple layers to the problem. Sometimes people are dealing with some really complex issues in their personal lives. And then you start layering on the changes we’re going through in health care, and the complexity of the patients we’re caring for, and all of that together begins to create the issues of burnout and resilience.
At the system level, we should provide employees access to counselors—financial counselors, addiction counselors, grief counselors, whatever they need.
But there are simpler things that can help, too. At Duke, we developed a course where we taught faculty and staff to write down three good things they did each day, before they went to bed. Those who did that every night were more resilient. We all tend to focus on what went poorly and forget about what went well. There are incredible things that happen every day at our hospitals. People shouldn’t lose sight of the difference they’ve made.
How did you gain your leadership skills?
I started at Duke in 1985 as a staff nurse in oncology. Then I got my MSN and I became a clinical nurse specialist. During that time, I was asked to lead an in-patient unit, which was a big deal back then.
What’s interesting is that I didn’t raise my hand and say, “Pick me.” I was told. And I look back on that story and I realize that the person who pushed me [supervisor and mentor Brenda Navigon] saw something in me that I didn’t see in myself. … When I look back on my career, there were incredible mentors who touched every aspect of my life: they taught me finance, revenue cycle, and a whole cadre of other skills outside of nursing that I needed to be successful.
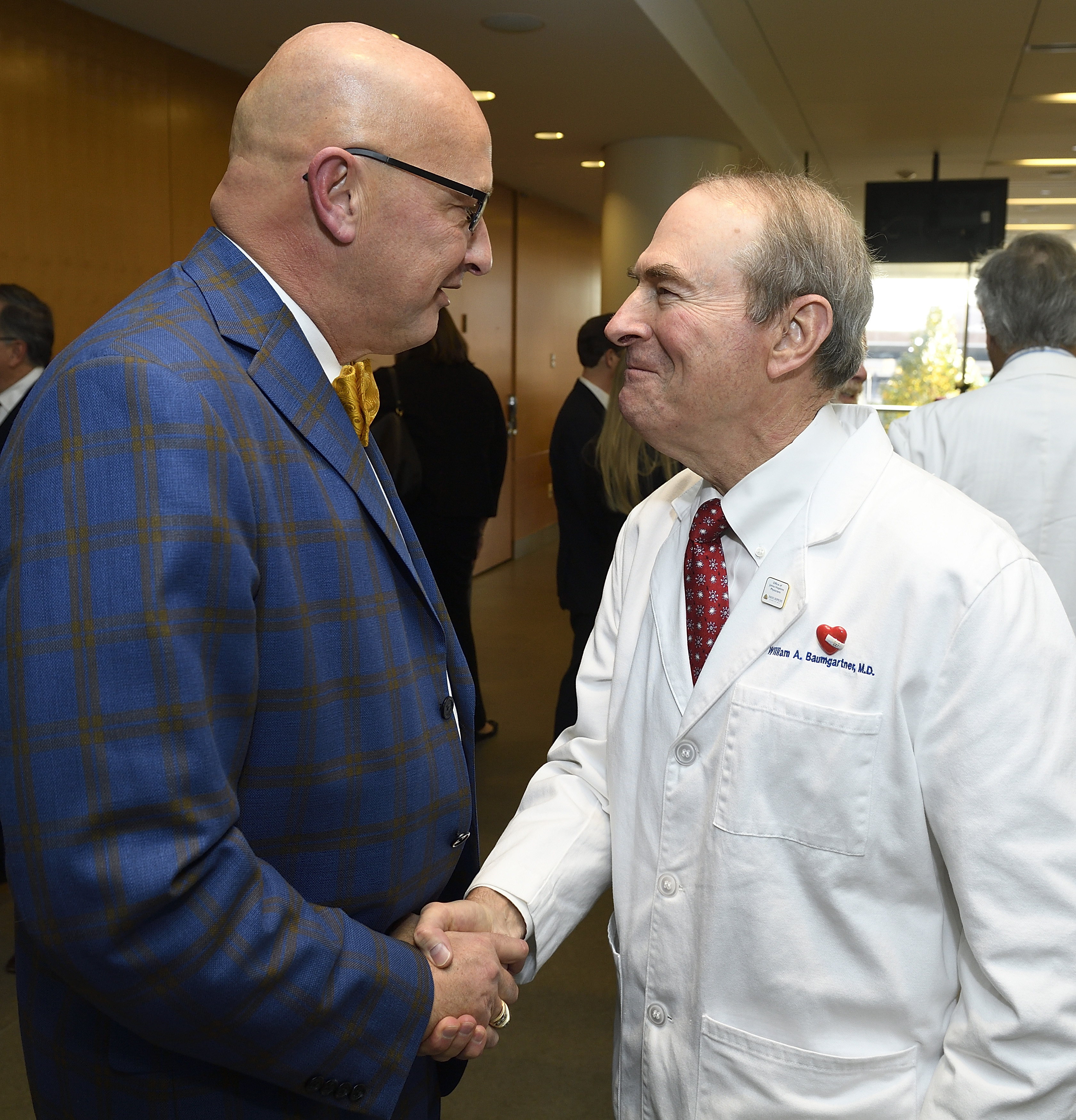
What inspires your sense of fashion?
[laughing] I didn’t know I had one… I have always loved bright colors. And I have always loved the color blue especially. The bow ties have been a signature piece for me. They’re just fun. This one [pale blue decorated with pink crabs] was a gift from the people at Duke who helped me develop a year-long leadership program for people from all disciplines. They thought I’d like some Maryland crabs.
What else do you like about Baltimore?
It has all the things that attracted me to Durham [North Carolina]. Both are foodie towns; both embrace the arts and the diversity of their people.
But there are other—less savory—parts of Durham and Baltimore. We need to partner with the city: help its leaders think through its health care needs but also partner with them around violence, which isn’t much different than in Durham. We accomplished a lot in Durham by partnering with the mayor and the City Council. … Baltimore has so much opportunity. It really does; it’s a great city.

 Wald Center Returns to Lead Community Care
Wald Center Returns to Lead Community Care A Letter from Deborah Baker: The Role of Your Career, Right Here
A Letter from Deborah Baker: The Role of Your Career, Right Here COVID and Nursing: Where to from Here?
COVID and Nursing: Where to from Here? From the Dean: Let’s Drive the Conversation on Health, Policy
From the Dean: Let’s Drive the Conversation on Health, Policy All Together Now!
All Together Now!







