Sibley Hospital fine tunes pediatric code blue emergency response through monthly simulations
There’s little time for staff to prepare and even less time to think when code blue is called due to pediatric cardiac arrest. Teamwork can mean the difference between life and death. And teamwork takes practice.
“Although things are done correctly [most of the time] during code blue situations, the process often seems ‘clunky.’ There is room for improvement when it comes to code blue preparedness in all hospitals,” explains Jennifer Abele, MD, Sibley’s Emergency Department medical director, who spearheads the simulations at the DC hospital.

Photo by Jim Burger | All available Sibley medical professionals are called upon once a month to perform back-to-back simulations on a manikin displaying symptoms of cardiac arrest. The code blue simulations may have already saved one baby’s life.
Therese Pearrell, MSN, RN, couldn’t agree more. “Pediatric code blue emergencies are low-volume, high-risk situations, and there’s a lot of low-hanging fruit when it comes to pediatric emergencies and code competency. Working together repeatedly is what enables us to quickly remedy code blue situations with precision in a way that no self-learning packet could ever teach.”
Sibley began code blue simulations–designed to (without notice) quickly summon all staff and emergency equipment–in May 2013. From nurses and respiratory therapists to anesthesiologists and even hospital chaplains, all available medical professionals are called upon once a month to perform back-to-back simulations on a manikin displaying symptoms of cardiac arrest. Meanwhile, participating nurses (three per simulation) have their shifts covered, so human patients aren’t left unattended.
“A simulation is performed just like an actual emergency situation,” says Abele. “The element of surprise is what keeps us on our toes. … Everyone responds quickly and willingly.”
“As medical professionals, we’re used to studying and preparing for what’s ahead,” Pearrell adds. With these exercises, “The lack of advance notice is the key ingredient. The simulations are the time to make errors. Making the wrong moves [when there is no danger to an actual patient] makes for better recall” during an actual emergency.
“We have learned so much about working together,” Abele says. “Learning to work as a team has helped this transcend beyond peds to adult cardiac arrest patients. It’s truly the best practice out there.”
Abele puts it in perspective: “We’re like an orchestra that needs to practice regularly for the big performance, so everyone can play their part in harmony.”
She recalls a note from the grateful parents of an infant saved during in actual code blue in August, an inspiring reminder that code blue simulations do more than save the life of the victim. They affirm the reality of what hard work can mean.
“Thank you … and thank you a thousand times again.”

 Help on Diabetes in Schools
Help on Diabetes in Schools DAISY Awards Spring 2023
DAISY Awards Spring 2023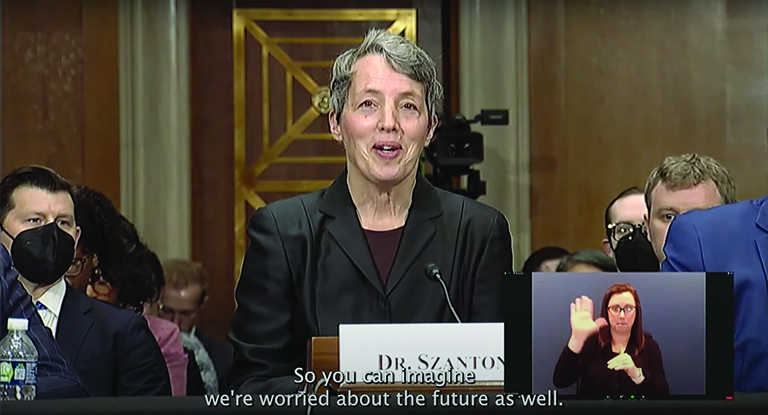 Class News Spring 2023
Class News Spring 2023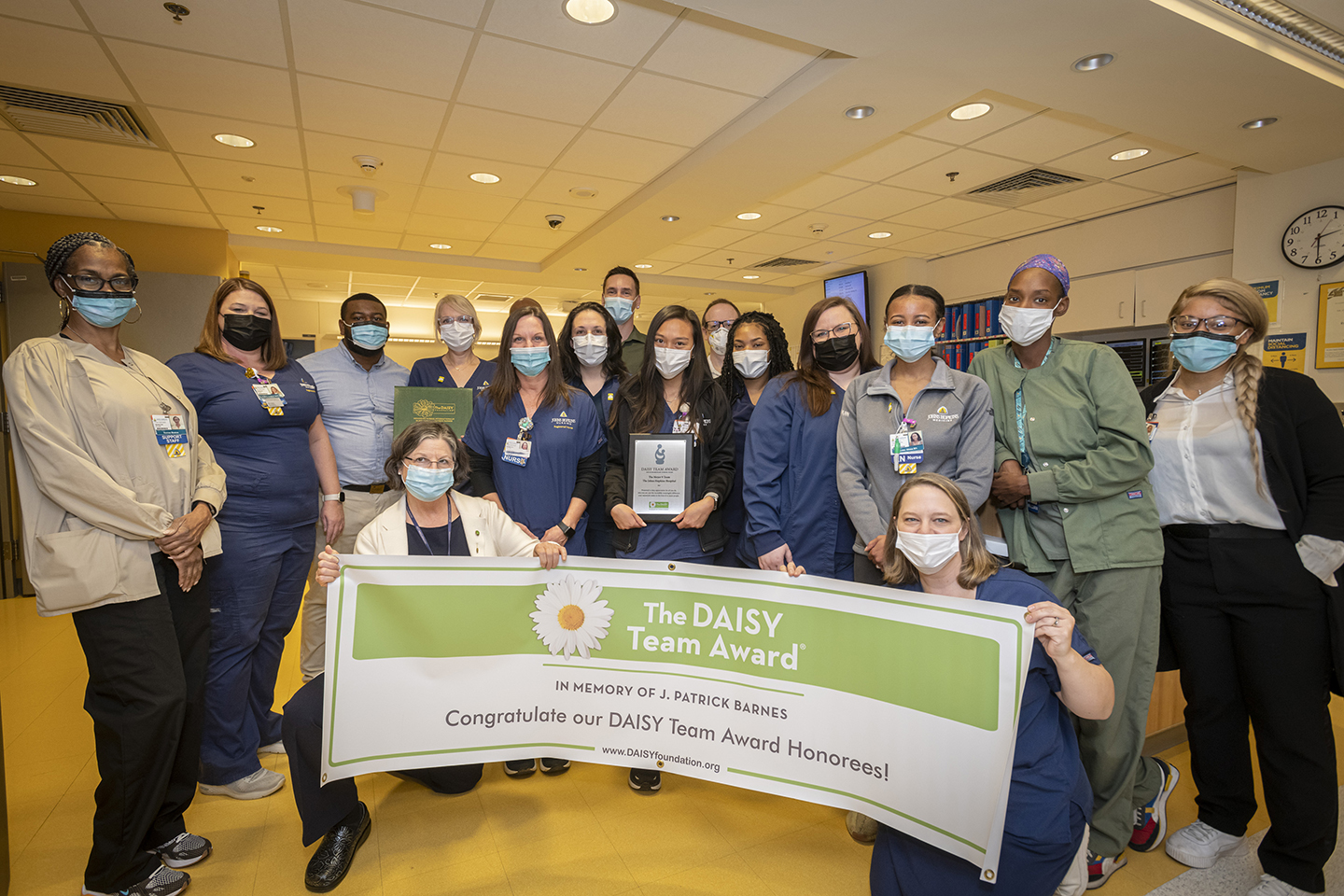 DAISY Awards
DAISY Awards Certifiably Awesome
Certifiably Awesome







