National curriculum survey, ‘a game changer,’ validates value in simulation
The patient, a middle-aged male, complains of severe chest pain. His mouth is drawn into a grimace; his skin is pale and clammy. A quick check of his vital signs reveals an elevated pulse, and the medical team strongly suspects a heart attack.
The student nurse:
a) Is asked to leave the room
b) Observes the action from the corner
c) Helps under the direction of her clinical advisor
d) Takes control of the situation
The correct answer? D, at least it is in the Johns Hopkins School of Nursing (JHSON) simulation lab. There’s no penalty, though, for answering A, B, or C; after all, those answers reflect the clinical experience of most nurses currently in practice. If a patient develops an acute complication during a clinical rotation–and that’s a pretty big if, as complications are by definition unpredictable–students are likely asked to leave the room, limited to the role of a bystander, or allowed to help in a very small, very supervised way.
In the JHSON sims lab, though, students guide a patient’s care. They obtain an EKG, get a “pulse ox” (a noninvasive reading of blood oxygen level), assess the patient’s pain, and notify the doctor. They keep an eye on the patient’s condition and respond appropriately when, say, atrial fibrillation occurs. They then stabilize and prepare the patient for transfer to a higher acuity setting.
They get to do those things because the “patient” is actually a high-fidelity manikin, capable of sweating, speaking, and responding to student interventions. The use of manikins (and, occasionally, actors) allows student nurses to safely perfect their skills in low-risk simulations before being called upon to respond in high-intensity, high-risk, real-life situations.
“In simulation, we put students in the role of the nurse,” says Sandy Swoboda, MS, RN, FCCM, a simulation education and senior clinical research coordinator with the Johns Hopkins schools of Medicine and Nursing. “They think as the nurse. They are making decisions independently with the knowledge they have, and if they go down the wrong pathway, that’s OK, because it’s a safe learning environment. If they make a mistake, they’re not going to harm a patient.”.

Emily Vaughn (left) and Alexandra Valencik treat a “patient” in the simulation lab.
The Rise of Simulation
JHSON has long believed in sims. Now there’s proof that it works. The National Council of State Boards of Nursing (NCSBN) National Simulation Study recently reported that students who receive as many as half of their clinical hours via simulation do as well on their nursing boards and in practice as peers who complete a traditional clinical experience.
Traditionally, nursing students have learned at patient bedsides. But in recent years, obtaining high-quality clinical experiences for student learning has become increasingly difficult. “Clinical sites are getting harder and harder to find,” says Pamela Jeffries, PhD, RN, ANEF, professor of nursing and vice provost for digital initiatives at Johns Hopkins University. In some urban areas, competition for clinical sites is fierce, and some rural areas don’t have enough healthcare facilities to accommodate students. Furthermore, rules designed to protect patient safety (and hospitals from liability) have limited what students can and cannot do in clinical environments. Some healthcare facilities no longer allow students to give medications.
Nurse educators also recognized the need to provide students with a broad array of experiences, one that can be difficult to meet in clinical settings where student experiences are limited by patient care requirements. Most students, for instance, never get the chance to witness or assist in a birth, much less care for a woman who is hemorrhaging post-partum.
Before the advent of high-fidelity manikins, it was difficult (if not impossible) to simulate such dynamic healthcare scenarios. Simulation, if it was used at all, primarily allowed students to practice skills in a static environment. In the 1990s and 2000s, though, increasingly sophisticated, computer-controlled manikins made their way into nursing simulation labs, and students and instructors quickly realized that these devices could be used to simulate actual patient encounters.
Simulation, says Cynthia Foronda, PhD, RN, CNE, assistant professor of nursing, is “a guaranteed way to give students many experiences. The sky is really the limit in terms of what can be taught and learned.” Instead of worrying about clinical availability, nursing instructors can create simulation experiences that put students in an active vs. a passive role.
Illustration by Harry Campbell
Simulation as a Substitute
Perhaps not surprisingly, given the difficulty of securing clinical sites and experiences for students, the number of schools of nursing using simulation to teach students has increased dramatically. And as schools began to realize the utility of simulation, some began petitioning their state boards of nursing, asking to substitute simulation time for a portion of students’ clinical time.
While the anecdotal evidence seemed solid, there was little concrete evidence–and much skepticism–that simulation experiences could replace real-life clinical encounters. The NCSBN study was designed to carefully analyze the effectiveness of simulation in nursing education. It is the first large,
randomized controlled study to compare the education and preparation of students who complete their clinical experiences in traditional settings to students whose clinical experience includes a combination of simulated and traditional clinical encounters.
The study followed more than 600 nursing students from 10 different institutions over two years. One-third of the students received 25 percent of their clinical education in a simulated environment. One-third received 50 percent of the clinical education via simulation. The remaining third, the control group, had traditional clinical experiences; no more than 10 percent of their clinical time was spent in simulation.
JHSON participated in the study, and educators and researchers Swoboda and Maggie Neal, PhD, RN, served as co-coordinators of the study at Hopkins, as well as skeptics.
“We both went in saying, ‘We don’t believe that simulations can possibly replace the clinical environment,’ ” Neal recalls, yet the study ultimately proved them wrong. The NCSBN study shows that students who receive up to half of their clinical experience in simulated environments are as knowledgeable and competent as students who complete their clinical experience in the traditional manner.
Jeffries, a co-author of the study, calls it “a game changer.”
“There was not a lot of evidence out there looking at the science and pedagogy of learning through this kind of experiential learning,” Jeffries says. “Now, though, we have this huge evidence base to show that students do learn in simulation.”
Simulation at JHSON
The study results are welcome news to students and staff at JHSON, many of whom realized the value of simulation through the school’s participation in the NCSBN study. Despite her initial doubts, Neal now considers simulation an effective and efficient way to teach students clinical skills and critical thinking.
“In a clinical practice setting, faculty usually have somewhere from six to eight students to supervise, and you can’t begin to see what’s going on with each of those students in a clinical environment on a daily basis,” Neal says. “In a simulated environment, I can guarantee that students are competent because I can make everybody do a simulation scenario and can see each of them.”
Nursing students and staff have access to four fully outfitted simulation rooms, and students begin participating in simulated scenarios during their first nursing class. Some, such as the heart attack scenario described at the beginning of this article, use manikins. Others, such as a psychiatric interview with a patient with schizophrenia, use actors. In all cases, students have the opportunity to take on and inhabit the role of the nurse.
“What’s great about a simulation is that it flows based on the students’ interventions,” Foronda says. “If a student forgets to apply oxygen, the patient’s O2 saturation will drop until the student notices and intervenes; we can make those changes to the manikin’s vital signs.”
And because the experience is simulated, staff can allow students to progress through an experience without stopping to protect patient safety. Later, students and staff discuss the experience in a debriefing session, with each person called on to respectfully share observations.
The debriefing session, often twice as long as the simulated encounter, is an essential part of the success of simulation learning, Swoboda says. “We go through a very structured debriefing process. We engage students in a discussion; we give them a little information and then draw out from them what they’ve learned. We help them make connections between what they’ve learned in class, what they learned in simulation, and what they learn in clinical.”
“What’s great about a simulation is that it flows based on the students’ interventions. If a student forgets to apply oxygen, the patient’s O2 saturation will drop until the student notices and intervenes.”
– Cynthia Foronda, PhD, RN, CNE
Simulation days are intense. Currently, eight hours of simulation are considered equivalent to eight hours of traditional clinical, but whereas students typically care for one patient (and spend lots of time reading charts and observing) during clinicals, sims students participate in two or three scenarios in the course of an eight-hour day. “With sims, they’re working the whole time they’re here,” says Nancy Sullivan, DNP, RN, JHSON sim lab director.
The Future of Sims
At present, JHSON students receive about 18 percent of their clinical education in a simulated environment, and that percentage is unlikely to change in the near future–despite the NCBSN study–because of logistical challenges. “Simulation is resource-intensive,” Swoboda says. High-fidelity manikins cost more than $70,000 apiece, and the amount of simulation education an institution can provide is limited by the number of manikins, faculty, and simulation suites available.
Still, nursing educators expect simulation to play an ever-larger role.
“I personally think simulation is going to get bigger and bigger and bigger,” Sullivan says, calling it an ideal way for healthcare personnel to practice low-occurrence, high-risk scenarios, such as an Ebola outbreak. She expects simulation to play a larger role in the education of graduate-level nursing students as well.
Simulation may also pave the way for interprofessional learning. Foronda hopes to eventually use virtual simulations to “span traditional boundaries and foster interprofessional communication.”
“Right now,” she says, “it’s very challenging to find space to facilitate interprofessional simulation. I’d like to foster virtual simulations that have physician students, pharmacy students, and nursing students interacting in a virtual world.”
Meanwhile, educators with experience in simulation are sharing insights and best practices with other nursing faculty. Neal coordinates the Maryland Faculty Academy of Simulation Training (MFAST), a group that’s teaching faculty how to write, facilitate, and debrief simulation scenarios. Jeffries serves as president of the Society of Simulation in Healthcare, a group that shares information and conducts research regarding simulation.
Jeffries and Sullivan predict that future nursing students may eventually be required to participate in standardized simulation scenarios deemed an essential part of nursing education. Some schools, Sullivan says, are even moving toward requiring students to demonstrate proficiency in simulation before allowing them to handle certain patient scenarios in real-life clinical settings.
“In simulation, we give our students experience that leads to increased comfort when they encounter scenarios in the real world,” Sullivan says. “They can build on their experience much more readily as a real nurse if they’ve already seen that situation in a simulated scenario.”
REAL-LIFE EXPERIENCE BEHIND THE SIMS
 Nancy Sullivan’s mother was no dummy.
Nancy Sullivan’s mother was no dummy.
“I always wanted to do what my mother did,” says Sullivan, daughter of a nurse and herself a 2013 graduate of the Hopkins DNP program.
“I thought it would be really cool to go to a nursing diploma program, so I could live in a dorm with other nursing students, right on the hospital grounds,” Sullivan recalls. “But I was very lucky because my mother was insistent and said, ‘No, you need to get your degree.’ Of course, that turned out to be a very good idea.”
Having a degree in nursing – at a time when few others did – ultimately allowed Sullivan to serve as a clinical instructor, lecturer, and clinical coordinator. She brings that experience, and 30-plus years as an emergency/trauma/critical care nurse, to her new role as simulation lab director.
“My role is to take our simulation lab into the future,” Sullivan says. “Our students love to learn, and it’s fun to watch them make connections and get more comfortable with what they’re doing. It’s a privilege to be able to support them throughout their education.”


 From Health at Home to ICU, Pediatric Nurse Practitioners Talk About the Care Continuum
From Health at Home to ICU, Pediatric Nurse Practitioners Talk About the Care Continuum Heart Health in Native Populations
Heart Health in Native Populations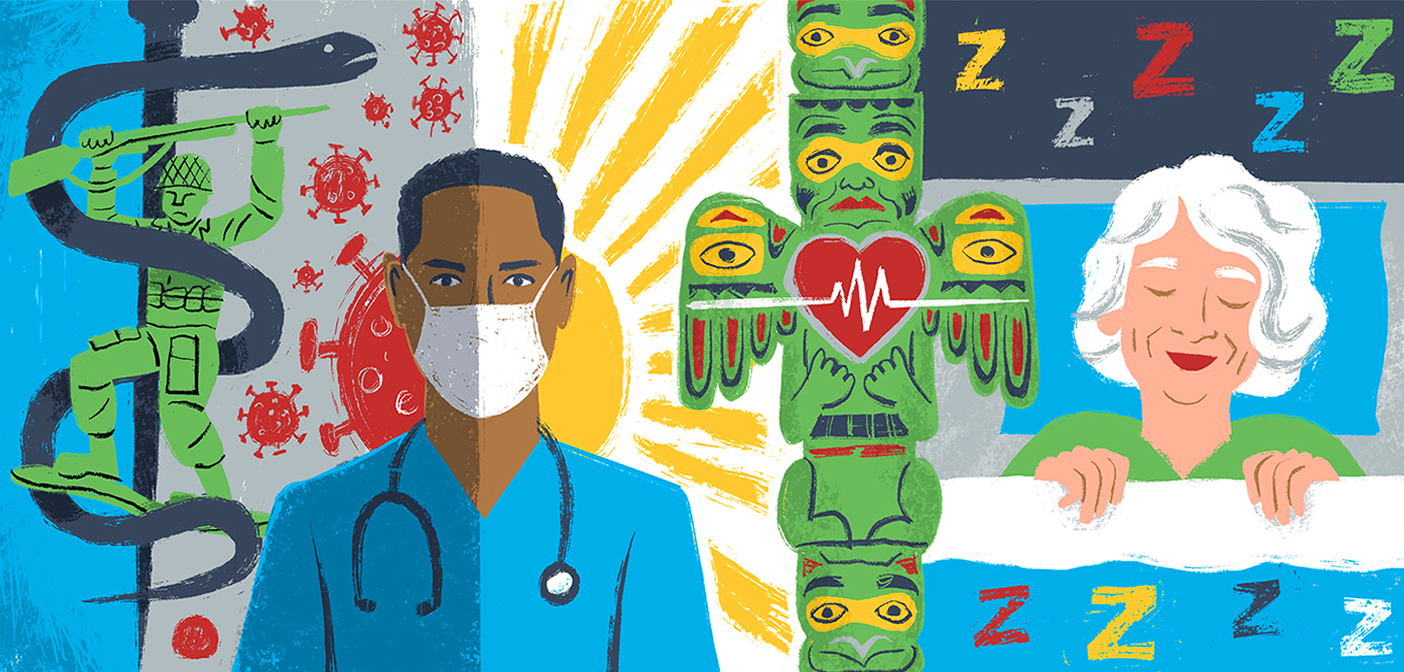 Summer Research Roundup 2023
Summer Research Roundup 2023 Appreciation: Fannie Gaston-Johansson
Appreciation: Fannie Gaston-Johansson Sky’s The Limit
Sky’s The Limit