My last pediatric clinical is next week and I’m sad to see it go. After not getting the floor I wanted at Hopkins, Kennedy Kreiger Institute (KKI) was the one of the few clinical sites still open and I quickly signed up for it (I said to myself, “I think I heard good things about this place…”). I got so lucky. It’s a treat having the entire hospital to yourself vs just one unit on a floor at most clinical rotations. At KKI, the first floor is the Neurobehavioral Center, therapy center, behavior center, school, physical therapy (PT) and occupational therapy (OT). Second floor is the PT spinal gym and feeding program. Third floor is our home base, the inpatient unit. The 4th and 5th are offices, where we do our morning quick conference. With all of this, me and my clinical buddies, all 6 of us, get to run around to all the floors bringing our patients to and from therapies.
KKI is a full service hospital. The kids here in between therapy sessions still get to go to school or practice a musical instrument. They are all also followed closely by a behavioral psychologist. The kids are amazing – a big group of fighters. They still have their good days and bad ones, but overall they work so hard to regain their strength. Many of the kids we get are a little older, about 13+, and the backgrounds are post car accidents, traumatic brain injuries, and surgeries for spina bifida, cerebral palsy, etc. As complete care nurses, we get the kids up in the morning, assess, give meds, help them get ready, and then out the door by usually 8:30AM for therapy. When there’s medications due at 10AM, we check where the kids are at, be it school, therapy, etc, and pull them aside for a second to make sure their meds are on time. When there’s a tube feed or water bolus during PT, no problem, we got this.

We’ll go to PT, wait until the therapist brings our patient down from a harness. We’ll pull the patient aside and into a small treatment room, and connect their feed or give them their bolus in private.
Lunch time is my favorite time to be with the patients. It’s easy to bond over food, even “bootlegged” hospital food as one of my patients called it. After all the running around we do in the morning, at lunch we get to sit with these kids and talk. I’ve learned that I enjoy working with adolescents. Maybe it’s that I am young enough to be more like an older sister to them that makes them more willing to talk or maybe it’s that I don’t take their quips and attitudes personally that makes me work well with them. It’s fascinating to see the developmental stages in all the children too, especially the kids with chronic illnesses who may have delays in cognitive development. I always heard “there’s psych in all types of nursing” and cannot agree with that in my previous adult health experiences but in pediatrics, it’s true.
My clinical group is also making my experience here one of the best I’ve had. We’re six very different women, but all of us get along and always have each other’s back. We all enjoy healthy food (i.e. kale salads and zucchini muffins) and for the past couple weeks have been trading recipes and sharing homemade goodies. Our instructor rounds the rest of it out perfectly. I’ll admit, on the first day, her fervor for teaching and strictness got me a little scared. But once we were on the floor, we all knew that we could go to her with anything we needed help with and she’ll guide us through the process stress free. This week we’re going to her office to share some home cooking (brought by us students!), burn incense, and meditate. Yeah so we’re in for a little new-age experience, but considering how intense this ABSN program is, some meditation is exactly what we need right now.
For the first time since my psych rotation I’ve been coming home excited to tell my husband via Skype how my peds clinical day went (all HIPAA rules enforced, 🙂 of course).
Maybe this is where I’ll end up. There’s lots of Transitions talk going on, not many answers, but I’ll definitely update once I have some sort of plan in mind.
Lastly, let me show you how I’ve been managing this (mild) winter:

Seared Romaine Salad
(serves 1 hungry nurse status post clinical, or 2 normal appetites)
Ingredients:
- 1 head of romaine lettuce
- 1/2 cup chopped veggies (I used onions and tomatoes in this picture, any would do)
- 1 clove of garlic, minced
- 1/2 tbsp of olive oil
- 1 tbsp salad dressing of choice
- Salt, pepper
Wash and dry your lettuce very well, then cut it in half lengthwise. Season the cut sides of the lettuce with salt and pepper. In a skillet on medium heat, cook your veggies in 1 tsp olive oil. Add salt, pepper, and cook for about 5 minutes, until the veggies are fully cooked. Set these aside on a plate. With the skillet still hot, add the rest of the oil and garlic and saute for a minute. Carefully place the romaine lettuce cut side down onto the skillet and press down for 30 seconds. Flip the lettuce over and press down lightly for another 30 seconds. Put your lettuce on a plate, top with the veggies you already cooked and then the olive oil and garlic mixture. Drizzle the salad dressing on top and serve with a fork and serrated knife.
I ate mine with a veggie patty and some potato chips (healthy huh?), and was a little worried about cooking lettuce, but it was super tasty and I’ve made this salad with many different cooked veggies and salad dressings. They’ve all been winners. The oil, garlic, salt and pepper wilt and flavor the lettuce just at the center, leaving the rest of the salad fresh and crisp. Let me know if you try this out, hope you like my new winter take on salad!
 Help on Diabetes in Schools
Help on Diabetes in Schools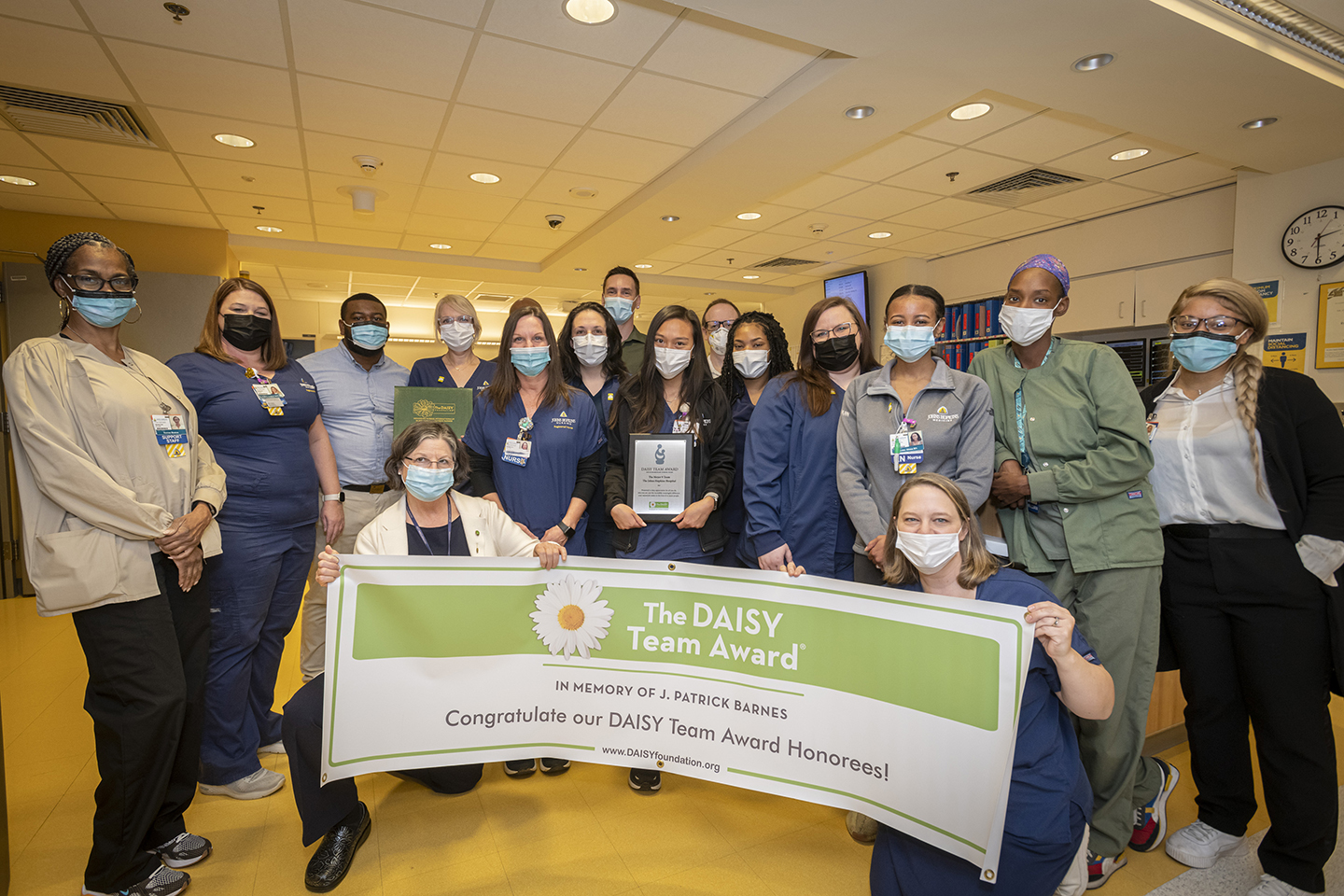 DAISY Awards
DAISY Awards What Is a Hopkins Nurse? Raji Koppolu
What Is a Hopkins Nurse? Raji Koppolu Scholarly Publications July 2016 – June 2017
Scholarly Publications July 2016 – June 2017 Ready to Roll
Ready to Roll







