Despite codes of conduct and zero-tolerance rules, disruptive workplace behavior happens. People become sarcastic, demeaning, or verbally abusive. Others gossip or form exclusive cliques. Sometimes, incivility and psychological aggression can explode into physicality. As workplaces, hospitals aren’t immune from this kind of disruptive clinician behavior; nor are nurses or other healthcare team members who work there.
That’s where Hopkins nurses Jo M. Walrath, PhD, MS, RN; Deborah Dang, PhD, RN, NEA-BC; and Dorothy Nyberg, MS, RN, enter the picture. They’ve been exploring the causes of, reactions to, and impact of hospital-based disruptive behavior through a series of focus groups with almost 100 nurses working in an acute-care hospital. Reporting on these structured interviews in “Hospital RNs’ experience with disruptive behavior,” Journal of Nursing Care Quality [online, November 2009], the researchers give voice to nurses’ experiences with disruptive clinician behaviors.
Walrath, an associate professor at the Johns Hopkins University School of Nursing, says, “Our exploration provides evidence that disruptive behavior can affect not only the safety of patients but also the cohesiveness of the healthcare team and the long-term health of the nursing workforce.”
The research team created a taxonomy that synthesized 168 different disruptive behaviors into three key categories: incivility, psychological aggression, and physical violence. The most frequent adverse behaviors were found to be triggered by issues related to personal char-acteristics, stress, fatigue, or competency.
According to Dang, Director of Nursing at the Johns Hopkins Hospital (JHH), “Disruptive behavior is so ingrained in interprofessional relationships, nurses often don’t recognize behaviors as disruptive.” That may explain why, when confronted by rude, insulting, or condescending behavior from peers, staff, physicians, or administrators, many nurses do not speak up, despite their longstanding role as patient advocates. Some hunker down; others choose to leave. Much can and must be done to promote more emotionally healthy workplaces for nurses, notes Nyberg, a program coordinator at JHH.
Walrath observes, “Because disruptive behavior can fracture the relationships that make up the healthcare process, it must be recognized by clinical care leaders, openly discussed and equitably addressed for the safety of all, particularly for that of our patients.”

 Sea Change for DNP Student
Sea Change for DNP Student Lateral Violence in the Workplace
Lateral Violence in the Workplace Do As I Do
Do As I Do Crucial Conversations
Crucial Conversations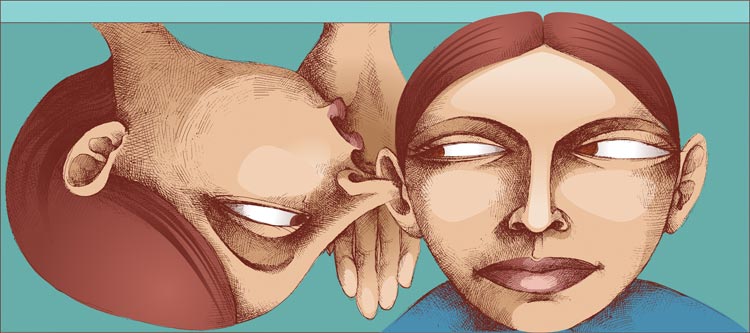 Loose Lips
Loose Lips







