How to manage patient pain
By Susan Middaugh
 Years ago, when nurse practitioner Yvonne M. D’Arcy broke her left leg, she “needed to learn everything” about managing her own discomfort—and thus began her new career specialty. Her mission: to alleviate pain among hospital patients, especially the elderly and adults who cannot speak for themselves.
Years ago, when nurse practitioner Yvonne M. D’Arcy broke her left leg, she “needed to learn everything” about managing her own discomfort—and thus began her new career specialty. Her mission: to alleviate pain among hospital patients, especially the elderly and adults who cannot speak for themselves.
As the nurse practitioner for pain management and palliative care at Suburban Hospital, D’Arcy, MS, CRNP, CNS, consults with 1,700 inpatients each year. Although patients may be admitted for a variety of reasons, pain is a common denominator for 99 out of 100 of them, she says. Among the most challenging to treat are surgical patients with chronic illnesses whose expectations about a pain-free outcome may be unrealistic. In many instances, readjusting those expectations is part of her job.
“There’s always something you can do to try to help the patient feel supported at a very difficult time in their lives,” said D’Arcy. In addition to medication, she shares her knowledge of other pain manage-ment techniques, including complementary therapies, which may be beneficial.
D’Arcy, a former high school English teacher, has authored or co-authored two books on pain management (four more are in the works), serves on the editorial advisory boards of three academic journals, and is a frequent speaker at nursing education conferences around the country.
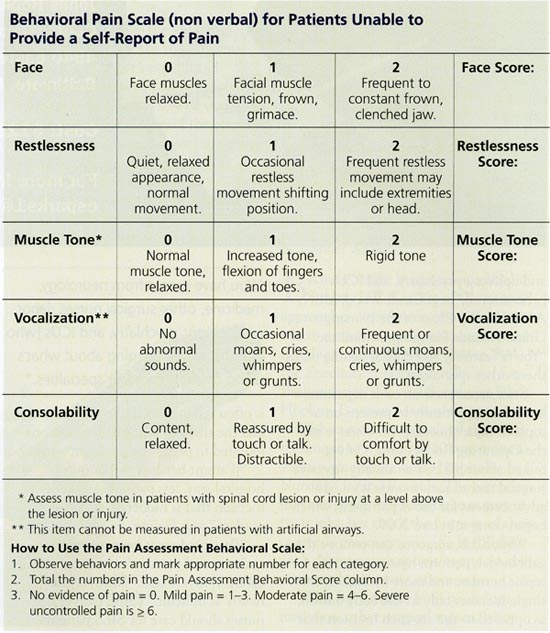
This October, as she has for many years, D’Arcy will lead a basic course in pain management and assessment techniques—particularly for elderly and non-verbal patients—for staff nurses in every unit at the hospital. In training staff nurses to be good diagnosticians, D’Arcy recommends using a behavioral pain scale to assess patients unable to provide a self-report of pain.
The diagnostic tool can be especially useful when family members of a non-verbal patient with dementia or aphasia, for example, resist increasing the patient’s dosage of pain medication. “Since the family knows the patient best, the nurses often do not feel comfortable disagreeing with the family or advocating for an IV with a heavier opioid,” D’Arcy said.
With training, she said, nurses become empowered to do what is best for their patients in pain.
 DAISY Awards Fall 2023
DAISY Awards Fall 2023 Appreciation: Fannie Gaston-Johansson
Appreciation: Fannie Gaston-Johansson Sky’s The Limit
Sky’s The Limit DAISY Awards Spring 2023
DAISY Awards Spring 2023 Fannie Gaston-Johansson Faculty of Excellence Program
Fannie Gaston-Johansson Faculty of Excellence Program







