A $1 million, two-year grant from the National Institutes of Health National Institute for Nursing Research (NINR) has been awarded to associate professor Gail Geller, ScD, MHS of the Hopkins Berman Institute of Bioethics, as part of an effort to build empathy and understanding among medical professionals who treat children with chronic health conditions.
A $1 million, two-year grant from the National Institutes of Health National Institute for Nursing Research (NINR) has been awarded to associate professor Gail Geller, ScD, MHS of the Hopkins Berman Institute of Bioethics, as part of an effort to build empathy and understanding among medical professionals who treat children with chronic health conditions.
Co-directed by Cynda H. Rushton, PhD, RN, FAAN, associate professor at the Johns Hopkins University School of Nursing (JHUSON), the study was one of only four percent that NIH funded among 20,000 Challenge Grant applications filed nationally. Seventeen other NIH Challenge Grants were extended to JHU schools.
With the grant, Rushton – who holds a joint faculty position with the Johns Hopkins University School of Medicine and serves as director of Johns Hopkins Children’s Center’s Harriet Lane Compassionate Care program – will develop and test innovative training methods that will include documentary videos of patients and families that are geared toward integrating palliative care into chronic pediatric diseases.
The project team also includes Mary Catherine Beach, MD, MPH; and Carlton Haywood, PhD, MA.
The effort, to be jointly run with the university’s Berman Institute of Bioethics where all four researchers are faculty members, is meant to sensitize the entire health care team that treats pediatric patients with either Duchenne muscular dystrophy (DMD) or sickle cell disease (SCD).
DMD and SCD are among the most common chronic, inherited, life-threatening diseases. But palliative care (defined as alleviating a patient’s symptoms and improving quality of life, regardless of whether the condition is curable) ultimately can improve the overall care DMD and SCD patients receive, Rushton and Geller said.
The researchers believe that the project will make caregivers — including neurologists, hematologists and other physicians; nurses; respiratory, occupational and physical therapists; genetic counselors; and social workers — “more compassionate and respectful, with a better understanding of what their [patients’] lives are like,” Rushton said. They will address caregivers’ emotions in treating such patients — the “tremendous feeling of inadequacy because of not being able to fix [what] is not fixable,” Geller added.
The recipient of the NIH grant was misidentified in an earlier version of this article. We regret the error.
 There’s a new cure for the deadliest strain of tuberculosis. So what’s that mean for the REACH Initiative’s HIV research in South Africa?
There’s a new cure for the deadliest strain of tuberculosis. So what’s that mean for the REACH Initiative’s HIV research in South Africa? The Vocabulary of Change: Leadership, Transition, Excitement, Celebration
The Vocabulary of Change: Leadership, Transition, Excitement, Celebration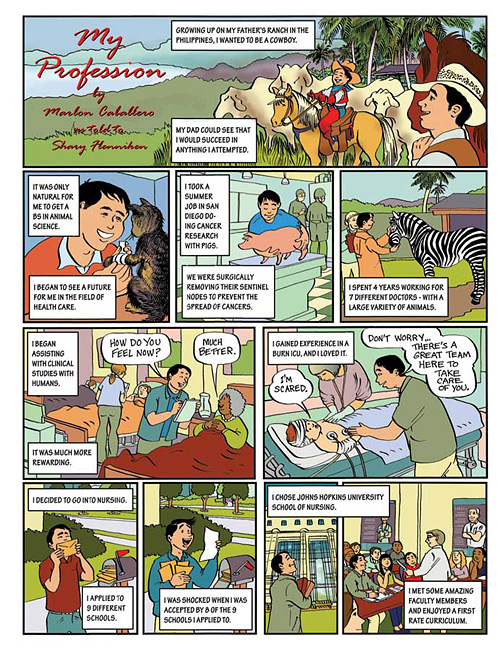 My Profession
My Profession Good Gourd! Dead Presidents Pick Halloween Best
Good Gourd! Dead Presidents Pick Halloween Best Second Opinion
Second Opinion